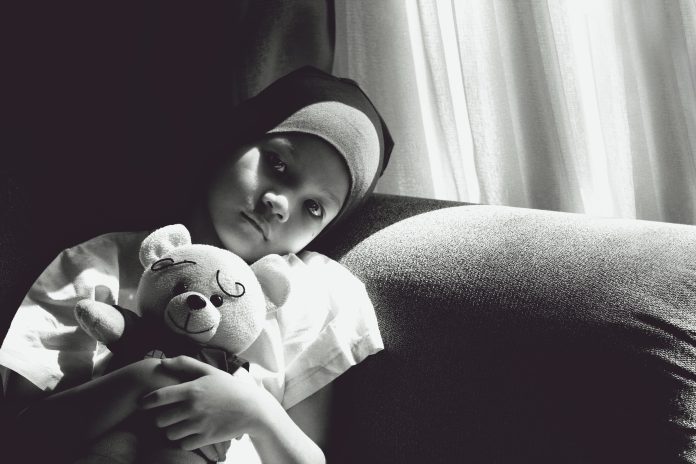
A novel treatment using supercharged immune cells appears to work against tumors in children with a rare kind of cancer, researchers reported Wednesday.
Nine of 27 children in the Italian study had no sign of cancer six weeks after the treatment, although two later relapsed and died.
The treatment — called CAR-T cell therapy — is already used to help the immune system fight leukemia and other cancers in the blood. This is the first time researchers have achieved such encouraging results in solid tumors, experts in the field said and raises hopes that it can be used against other kinds of cancers.
It’s too soon to call it a cure for neuroblastoma, a nerve tissue cancer that often starts in infancy in the adrenal glands near the kidneys in the abdomen.
Standard treatment can be intense, involving chemotherapy, surgery, and radiation, depending on the cancer’s stage and other factors. The children in the study had cancers that had come back or were particularly hard to treat.
Eleven children were alive when the three-year study ended, including some who only partially responded to treatment and got repeat doses of the modified cells.
“Those kids were all destined to die without that therapy,” said the University of Pennsylvania’s Dr. Carl June, a pioneer of CAR-T therapy who was not involved in the new research.
“No one’s ever had patients responding like this before, so we just don’t know what it’s going to look like a decade from now,” June said. “For sure, there are going to be more trials now based on these exciting results.”
CAR-T cell therapy harnesses the immune system to create “living drugs” able to seek and destroy tumors. T cells from the patient’s blood are collected and strengthened in the lab, then returned to the patient through an IV where they continue to multiply.
Six CAR-T cell therapies have been approved by the U.S. Food and Drug Administration for blood cancers. Some early patients have been cured.
But success in solid tumors has been elusive. The latest study was done by researchers at the Vatican’s Bambino Gesu pediatric hospital in Rome.
“They seem to have found a unique combination” to get the modified cells to multiply initially, then last a long time to continue their cancer-killing work, said Dr. Robbie Majzner of Stanford University School of Medicine, who was not involved in the new study.
Study co-author Dr. Franco Locatelli said they also added a safety switch to eliminate the cells if a patient had a severe reaction. When one patient had problems, they flipped the safety switch, showing that it worked, although later they determined the patient’s problem was caused by a brain bleed unrelated to the CAR-T cells.
Many of the children had a side effect that is common with CAR-T therapy — an immune overreaction called “cytokine release syndrome.” It can be serious; but was mild in most, the researchers reported.
They concluded that CAR-T therapy was “feasible and safe in treating high-risk neuroblastoma.”
The Associated Press Health and Science Department receives support from the Howard Hughes Medical Institute’s Science and Educational Media Group. The AP is solely responsible for all content.